Preventing Fraud And Abuse In Managed Care
CPI has also developed a managed care plan compliance toolkit with guidance to assist Medicaid managed care plans in preventing detecting and reporting Medicaid fraud waste and abuse CMS 2016a. 49 Issue 4 The role of the states in combating managed care fraud and abuse.

Medicaid Program Integrity And Current Issues Issue Brief 9385 Kff
Our papers are.
Preventing fraud and abuse in managed care. 853 West Washington Street. Prevent Detect Report MLN Booklet Page 5 of 23 ICN MLN4649244 January 2021 Medicare Fraud and Abuse. States have increasingly adopted managed care in response to Medicaid expenditures which have nearly doubled in the past decade.
State Health Care Expenditures favorable without amendment VOTE. Preventing Fraud and Abuse in Managed Care You need a critical thinking professional brain for the A paper you are here for. Under the FCA the United States may sue violators for treble damages plus 550011000 per false claim.
Another form of fraud that has become prevalent under discounted fee-for-service managed care is upcoding claiming for a service with a higher reimbursement than the service actually performed. For example managed care plans must maintain a system with dedicated staff charged with monitoring promptly responding to investigating and correcting internal compliance issues. 1 Preventing Fraud and Abuse in Managed Care Preventing Fraud and Abuse in Managed Care HSM 420 Managed Care Main Menu.
View Essay - Fraud and Abuse Managed Care from HSM 420 at DeVry University Chicago. Preventing Fraud and Abuse in Managed Care Never use plagiarized sources. Special Investigations Unit 7231 Parkway Drive Suite 100 Hanover MD 21076.
Call Toll-Free at 1-800-835-2556 TTY. Detecting and Preventing Fraud Waste and Abuse MVP Compliance Office 2019 5 Tampering with Public Records New York Penal Law 17520- 17525 A person may be found guilty of tampering with public records if he or. Below are some Examples.
This research paper focuses on health care fraud and abuse and more particularly health care fraud and abuse in Managed care in America. Talk to us and sit back and relax as we deliver just that right to you. A Serious Problem That Needs Your Attention Although no precise measure of health care.
Enforcement against health care fraud and abuse comes in the form of well-established legal mechanisms focused on penalizing such actions including 1 the False Claims Act United States Code USC section 3729 to 373357. A 2600 toenail. 247 telephone line that allows internal and external reporting.
Healthcare Fraud has a signific ant effect on Managed Care plans. 1 managed care contract procurement 2 marketing and enrollment 3 underutilization of services 4 claims submission and billing procedures 5 fee-for-service payments within managed care and 6 embezzlement and theft. To further fight the rising incidence of fraud and abuse in 1993 the Attorney General announced.
711 UPHP Compliance Hotline. In FY 2015 DOJ reported that 33 billion was recovered by the government related to healthcare fraud judgments and settlements Since 2007 Tennessee. Students can choose any topic from the book.
Preventing fraud and abuse fallout. Report all suspicions of fraud by contacting the JHHC Special Investigations Unit at. Preventing fraud and abuse in the Medicaid program COMMITTEE.
Get Your Original Essay on Preventing Fraud and Abuse in Managed Care Hire Professionals Just from 11Page Order Now Click here It is. CMSs guidelines identify six areas of fraud waste and abuse in Medicaid managed care. You may also report suspected fraud waste and abuse directly to the State of Michigan at.
We found that although managed care entities MCE and States are taking steps to address fraud and abuse in managed care they remain concerned about their prevalence. To help combat fraud and abuse the federal governments False Claims Act FCA of 1986 specifically targeted healthcare fraud and abuse. - 1 - HOUSE RESEARCH HB 1743 ORGANIZATION bill analysis 4102003 Delisi SUBJECT.
MANAGED CARE AND HEALTH INSURANCE PROJECT 20 of grade Students will choose a Managed Care Topic. As noted earlier managed care program integrity also includes many broader program oversight elements that at the federal level is the responsibility of the. 8 ayes Delisi Gutierrez Berman Crownover Deshotel Harper-Brown.
Pros and Cons of Managed Care In America. Third the Final Rule requires managed care plans to strengthen program integrity by implementing and maintaining programs and procedures to detect fraud waste and abuse. Instead of a small toenail fee one podiatrist claimed a 2600 foot operation for each nursing home patient.
Medicaid Fraud Control Units and managed care organizations in preventing identifying investigating reporting and prosecuting fraud and abuse in a Medicaid managed care environment and to better equip States with new 6. Meridith Seife a co-author of the report said We are concerned anytime we see evidence that managed-care organizations are not finding fraud and abuse and sharing it with states in a rigorous way And a 2020 GAO watchdog report found that at least 63 of MAOs encounter data is missing national provider identifiers data essential to tracking provider. Medicare Fraud Abuse.
Michael hfm Healthcare Financial Management 07350732 Apr95 Vol. The health care fraud is considered as a vital and observable aspect related to growing health care expenditures since there is no affirmative characteristic of it. Payment Integrity Department Attention.

How To Prevent Healthcare Fraud Best Practices For Government
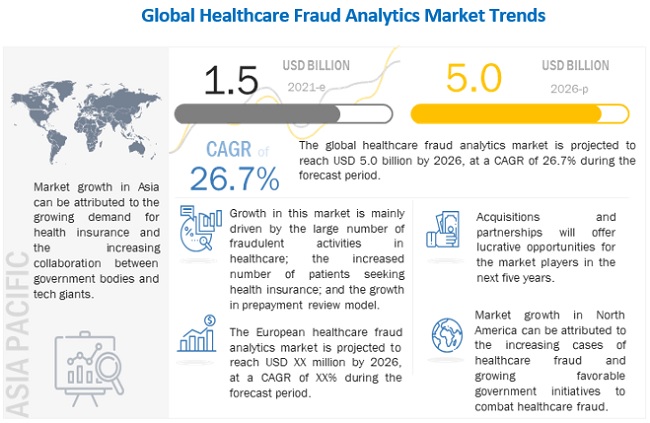
Healthcare Fraud Analytics Market 2022 2026 Size Share And Trends Marketsandmarkets

Healthcare Provider Fraud Detection Analysis Using Machine Learning By Anik Manik Analytics Vidhya Medium

Healthcare Whistleblowers Play A Critical Role In Stopping Fraud




Posting Komentar untuk "Preventing Fraud And Abuse In Managed Care"